How Opioids Made the Jump to Mainstream Use

The journey toward declaring not just palliative care, but pain relief itself, a basic human right occurred under the leadership of one of the pioneers in the pain field, Michael Cousins. Cousins was a master persuader. He represented the pain field in Australia over the entire span of his very long career, and probably had more influence on how pain was managed there than any other single individual.
As a young anesthetist in Sydney in the late 1960s, he undertook a postgraduate fellowship in acute pain management and worked for a while in McGill University, Montreal, which was pioneering the use of epidural pain relief. Between 1970 and 1974, he worked at Stanford University. During his time living and working in Canada and the United States, he interacted with other top pain specialists, Ronald Melzack, Patrick Wall, and John Bonica, which vastly broadened his horizons.
Cousins went back to Australia determined to build pain services and research in Australia much as Bonica was doing in the United States. He thus became part of the grand global scheme to improve pain management. His first task was to develop a multidisciplinary pain center at Flinders Medical Center in Adelaide, after which he moved back home to Sydney and developed another large multidisciplinary pain center at the Royal North Shore Hospital. Both centers became internationally recognized in their time. In 1979, he became the founding president of the Australian Pain Society, and in 1987, he became president of the International Association for the Study of Pain (IASP). He played a key role in the formation of an official relationship between IASP and the World Health Organization. He raised funds for pain research and education through the nonprofit community-based organization Pain Management Research Institute Ltd., which he founded in the 1990s. In 1995, he was made a Member of the Order of Australia for “service to medicine particularly in the fields of pain management and anesthesia.” By 1999, he had become the Founding Dean of the Faculty of Pain Medicine, and in 2005, he played a key role in the recognition by the Australian government of pain medicine as an independent medical specialty.

Influenced by his role in IASP, his palliative care colleagues, and his perception that acute pain management could be better, Cousins long held the view that pain relief, not just palliative care, should be considered a fundamental human right. He had been thinking and writing about the humanitarian aspects of pain relief since the 1980s. In his 1999 Rovenstine Memorial Lecture, he wrote:
In 1948, the United Nations Declaration of Human Rights said that “all persons are equal in dignity and rights and have the right to life, liberty and security.” One can obtain that document incidentally on the Internet, and you will find that it is implied that, with appropriate medical care, one is able to achieve the aim of some quality of life. Interestingly, the United Nations Declaration does not mention pain relief as being a human right. However, I ask you just to ponder what would be your priority list for basic human rights. Would you consider freedom from hunger, which has been discussed so extensively? Freedom from thirst? Peace without political or other persecution? Freedom of speech, press, religion, assembly, mobility? Certainly, these are all important. However, they are difficult to enjoy if one has unrelenting, severe pain. I put it to you that the relief of severe, unrelenting pain would come at the top of a list of basic human rights.
In 2000, he wrote in the Medical Journal of Australia, “Relief of acute, severe pain is a basic human right, limited only by our ability to provide it safely in the circumstances of individual patients.”
Frank Brennan and Daniel Carr were natural allies in Cousins’s quest to establish pain relief as a basic human right. Brennan was a palliative care physician/lawyer in Sydney who had published widely about the human rights dimensions of palliative care. Carr was an endocrinologist, anesthesiologist, and advocate leading the movement to embrace evidence-based acute pain management in the United States. The year 2004 was a banner year for their efforts. A “Global Day Against Pain” was launched by the WHO, in partnership with the IASP and the European Federation of IASP Chapters (EFIC). The theme of the global day was “Pain Relief: A Universal Human Right.” In an editorial with the same title published in the IASP’s journal Pain, Cousins, Brennan, and Carr wrote:
Failure to provide relief when this is available is a form of abandonment. In extreme cases it could be regarded as “torture by omission.” . . . The bio-ethical principle of justice can be used to assess the massive humanitarian and financial costs of severe pain and to argue to pain relief as a high social priority. A virtue ethics approach also places pain as a high priority. The current lack of a strong application of these principles to pain relief raises questions about the ethical foundations of current healthcare.
In time, Cousins went on to spearhead an initiative at IASP to write a declaration that the provision of pain treatment should be considered a fundamental human right. In 2010, he chaired the steering committee that developed an International Pain Summit in conjunction with the 13th World Congress in Pain held in Montreal. The “Declaration of Montreal: Declaration That Pain Management Is a Fundamental Human Right” was drafted during this summit; it was later approved by the IASP Council and published in 2011.
But by 2010, there was already a backlash against Cousins, Brennan, and Carr’s idea that access to opioids for the treatment of chronic pain was part of the fundamental human right to pain relief. In their 2004 article, they did not specifically call out opioids, but in 2007, when they wrote another more comprehensive article, “Pain Management: A Fundamental Human Right,” they did. In fact, they cited several initiatives in the United States to liberalize opioids for the treatment of chronic pain and called for liberalization of national policies on opioid availability. They suffered a backlash from others in the field who worried that their arguments were purely philosophical and not evidence-based, and that their framing of a right to opioids would result in opioid overprescribing.

By 2007, alarming data on rises in prescription opioid abuse admissions and death rates were coming out of the United States, and by the time the framers of the Declaration of Montreal met in 2010, there was caution about promoting opioids: The document itself was careful to promote neither access to pain “relief” nor opioids, but instead access to pain management. To pain specialists, “pain management” meant multidisciplinary pain care. But it did not mean much to primary care providers, who knew few pain management techniques beyond opioids.
Nobody could accuse Michael Cousins, Frank Brennan, or Daniel Carr of having any other than the highest motives for promoting opioid therapy for the treatment of distressing pain. They had humanitarian goals; they dedicated their lives to those humanitarian goals; and they labored under the belief of the time that when opioids were used for serious pain, they would rarely be addictive. But that belief was based on the experience that opioids used at the end of life or in hospital settings for short-lived pain are rarely, if ever, addictive. This belief was reinforced by the low rates of addiction in studies such as the seminal 1986 study by Russell Portenoy and Kathleen Foley, two other key early advocates of opioids for pain relief, which had been conducted by careful physicians in a controlled setting treating a subset of patients not generalizable to the general population.
But unfortunately, those favorable experiences did not extend to the wider population. As Portenoy and Foley said themselves, “the efficacy of this therapy and its successful management may relate as much to the quality of the personal relationship between physician and patient as to the characteristics of the patient, drug, or dosing regimen.” That proved to be a key element in what followed. Prescribers and patients alike began to struggle with what, other than a high pain score, was the right indication for opioids. Treating those with the highest pain scores selected patients with significant mental health and substance abuse comorbidities (who had been excluded from the randomized trials of opioids for chronic pain) for opioid treatment. Clinical experience went on to reveal that the opioid treatment did not help over the long term, and addiction rates were much higher than had been predicted.
In no country other than the United States have prescription opioid misuse, abuse, and death rates reached epidemic proportions. These problems increased in parallel with increased prescribing for chronic pain. More and more pain conditions were being treated with opioids using higher and higher doses. Prescription opioid misuse was called out as an epidemic in 2012, but this was only the first wave of the current opioid epidemic in the United States. The prescription opioid epidemic evolved into a heroin epidemic and then into the even more lethal fentanyl epidemic. But all these epidemics originated with the widespread prescription of opioids for pain.
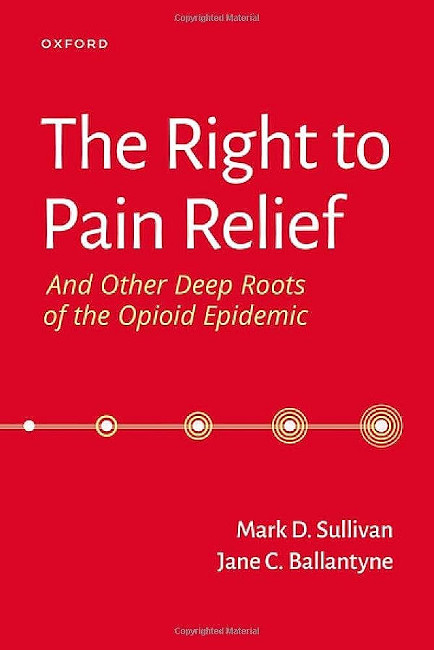
Author Bios:
Mark Sullivan, MD, PhD, is Professor of Psychiatry and Behavioral Sciences at the University of Washington. Jane Ballantyne, MD, FRCA, is Professor of Anesthesiology and Pain Medicine at the University of Washington.
They are the co-authors of The Right to Pain Relief and Other Deep Roots of the Opioid Epidemic, an excerpt of which is published here with permission.
Highbrow Magazine